 Information for Patients
Information for Patients
Information for Professionals
A journey from the past to the present
As early as in 1928 the first „Infektionshaus“, a hospital for infectious diseases, was opened on the site of the present hospital, mainly for patients suffering from tuberculosis. The site featured multiple buildings, called pavilions, with wide balconies providing excellent conditions for the treatment of the “white plague” as far as that was possible at that time.
At the end of World War II Delmenhorst’s population multiplied, so additional hospital buildings had to be erected. The introduction of antitubercular medication led to a decrease in patient numbers, but at the same time growing cigarette consumption and an occupational exposition to asbestos, especially in the wharves and the ports in the area of Delmenhorst, caused an overproportionally increasing incidence of pulmonary malignant tumors, such as bronchial carcinoma and pleural mesothelioma. Both trends resulted in a growing need for medical therapy of pulmonary diseases in Delmenhorst.

Josef- HospitalDelmenhorst, Lower Saxony (Germany); the oldest building opened in 1928.
On the 1st September 2003 the Clinic for Thoracic Surgery was opened, initially as part of the Center for General- and Visceral Surgery. Since the 1st of January 2007 it is the independed Center for Thoracic Surgery and Intrathoracic Vascular Surgery

Center for Thoracic Surgery, newest building, opened in 2008.
Presently the Center for Thoracic Surgery and Intrathoracic Vascular Surgery attends to about 620 patients (inpatients and outpatients) every year with an annual increase of 20%. In 2007 a total of 349 patients were given surgical treatment. Of these operations 38% were performed using minimal invasive techniques, 52% via anterior thoracotomy and in 10% a combination of minimal invasive technique with conventional procedure was applied, a new method developed in this hospital. The average stay was 7,9 days long with an intensive care treatment of 1,3 days (in case of extensive lung resections).
Complication rates were very low, the mortality rate for lobectomy was 0% in 2007 (average in Germany 1-4%), for pneumonectomy 0.3% (average in Germany 6-17%) and for more extensive operations including intrapericardial resections the mortality has been 0.9% (average in Germany 8-19%). The rate of general complications was 1,8% over all operations. The most common problem was a transient pneumonia following the operation.
Technical Requirements
The Center of Thoracic Surgery and Intrathoracic Vascular Surgery can dispose of all modern technical and logistical methods for diagnosis and surgical therapy, including computertomography (CT), magnetic resonance imaging (MRI), minimally invasive procedures, Laser- or Argon-Beamer carbonisation, bronchography and digital bronchoscopy. Patients with highly contagious diseases are cared for in a special unit for infectious diseases.
All other than pulmonary affections are specially looked after by an interdisciplinary network of internal, pneumological, cardiological and anesthesiological therapists. Severe conditions are treated by the team of our intensive care unit.
Modern, less invasive and lung tissue preserving techniques are applied not only in the treatment of pulmonary or mediastinal tumors but also of traumatic lesions, vascular surgery or congenital vascular anomalies (e.g. sleeve- or double-sleeve resection with vascular interpositions).
Parallel to the development of new surgical methods the logistics of patient care are our major concern. Patients can expect a date for acceptance in our hospital within one week after application. Diagnostics of suspect pulmonary foci and staging examinations will be performed within three days.
New developments, such as the “interventional thoracoscopy” and the surgery of intrathoracic neural lesions (e.g. idiopathic paralysis of the N.phrenicus) were introduced by our department.
Thoracic approaches via the side or the back (anterolateral or dorsolateral), which had frequently been used in the first centuries of thoracic surgery, are now abandoned in favour of an approach through the anterior thoracic wall between the 4. and 5. rip. This allows large resections although the wound is only about 10 cm long.
For minimally invasive operations the number of approaches was reduced from 3 to only 1 remaining. This approach is set up in the front axillary line through the space between the fifth and the sixth rip. It is used for a digital camera und for the operative instruments at the same time. This procedure reduces postoperative pain significantly. If necessary the same approach can be extended to ca. 4 cm for larger resections, a procedure called “interventional thoracoscopy”, allowing a combination of minimally invasive and conventional surgical techniques.
Benign tumors of the thymus gland can be removed using the minimally invasive procedure coming from the left side through the space between the 4. and 5. rip.
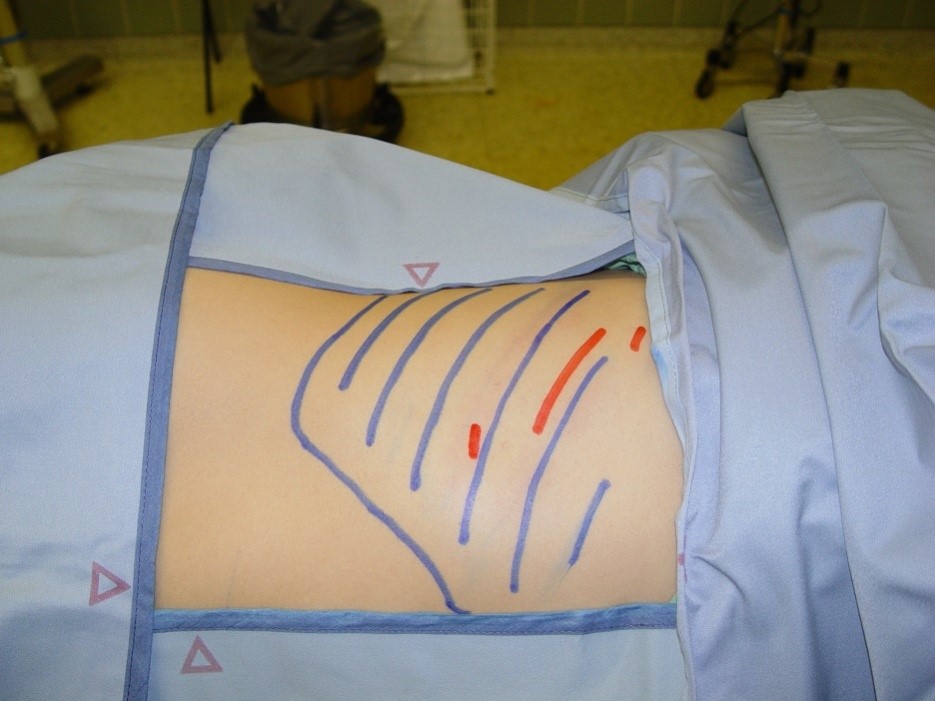
Pic. 3: Size and localisation of the skin cuts fort he performance of a thoracic operation using classical technique (blue marks) or combined with minimally invasive methods (red marks).

Pic. 4: Small wounds and cosmetically favourable approach to a lung operation (here a 26 year old patient, 21 days after the resection of destroyed parts of the lung).
Range of Operations
Operative procedures are performed on
- Children (5 years and older) and adults (regardless of age) suffering from
- Tumors of the airways, the lung or the mediastinum, such as:
- a. Bronchial carcinoma
- b. Metastasis
- c. Benign or malignant pleural tumors (e.g. mesothelioma)
- d. Benign or malignant tumors of the thymus gland
- Intrathoracic infections with empyema or abscess
- Residual effects of traumatic lesions
- Cysts or bullae (pulmonary emphysema)
- Residual symptoms of tuberculosis
- Congenital anomalies (e.g. bronchiogenic cysts, anomalies of blood vessels or lung tissue)
- Lesions and diseases of the trachea.
No operations are performed on
- Patients with cardiac diseases necessitating the use of a heart-lung-machine (e.g. cardiac bypass operations or cardiac valve implantations);
- Vascular Alterations of the central Aorta (from the heart to the branch of the artery supplying the left arm).
The routine implantation of peridural catheters (for the first 3 days) allows the efficient control of postoperativ pain by a continious spinal application of analgetic medications.
Special Surgical Techniques
Putrid Infections of the Pleura (Pleural Empyema)
Today the treatment consists of an operative debridement and extensive lavage using 15-50 liters of saline solution. Only in 2% a continious lavage over 2-3 weeks is necessary after the primary operation.
Sleeve-Resections
Sleeve-resections are indicated for the operative removal of tumors extending to the central origin of larger bronchi (lobar or segmental) or infiltrating neighbouring blood vessels. This procedure allows a sparing resection of lung tissue and has resulted in a decrease in the number of pneumonectomies.
Today lobar bronchial sleeve-resection is a standard procedure, but segmental sleeve-resections are reserved for special indications, such as the resection of bronchiectasy in pulmonary emphysema. Double sleeve- resections include bronchial and vascular sleeve-resections in one operation.
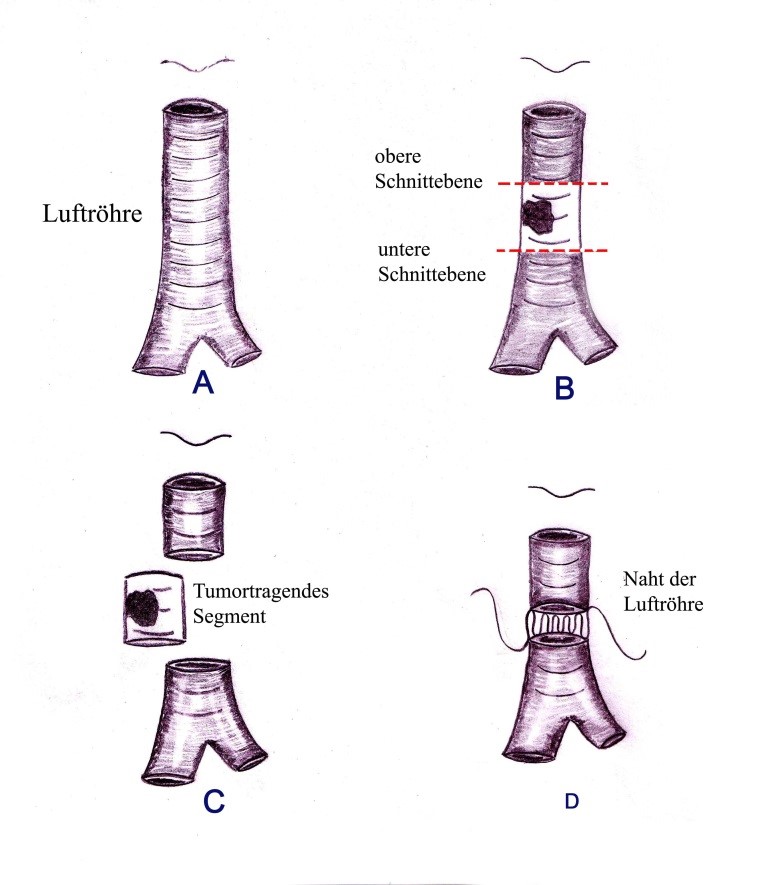
Example of the resection of a tumor of the windpipe. After the tumorbearing segment has been removed, the ends are united by using special sutures.
Suction Therapy
Drain tubes implanted during or before an operation allow the appliance of negative pressure to remove trapped or incoming air. Specially designed suction systems allow the application of up 120 mm Hg of negative pressure. In case of fistulas of the lung tissue a loss of 30% of breathing volume can be compensated using these systems. The application of fibrin glue or collagen fleeces is not necessary anymore.
Extensive lung resections
Intrapericardial operations as well as the replacement of large veins leading to the heart (e.g. Vena cava superior) are routinely performed. Veins are ligated including their base in the cardiac atrium and replaced by GoreTex-implants, Aortic sections are replaced by Dacron-bypasses.
A team of specialists is prepared to treat patients with all kinds of thoracic diseases:

Prof.HUST WuhanDr.med. Martin Teschner specialist for general, thoracic and vascular surgery and medical director of the Center for Thoracic Surgery and Intrathoracic Vascular Surgery
(e-mail: m.teschner@jh-del.de)

Frau Iris Martens, chief secretary of the Center for Thoracic Surgery and
Intrathoracic Vascular Surgery
Tel.: 0049/ 4221 – 994263; FAX 0049/ 4221- 994265.
Herr Dr.med. Matthias Esch
Specialist for general surgery and assistant medical director.

Dr.med. A. Müller, psychooncologist; specialist for the psychological assistance to patients with malignant diseases.

The nursing team of ward 31 (thoracic surgery)


Specialised and experienced in the care for patients of thoracic surgery: the nursing team of ward.

The team of the department for physiotherapy.
The clinic consists of three major parts: the new building housing three patient wards with spacious, comfortable rooms, modern sanitary facilities, TV and radio in every room.

Reception area of ward 31 (thoracic surgery).

Patient rooms, spacious and friendly, equipped with facilities for physically handicapped persons.

Lounge of ward 31 (thoracic surgery).
Secondly the north wing of the old building which was converted to a modern outpatient clinic, conserving the architectural details.

Outpatient clinic of the Center for Thoracic Surgery and Intrathoracic Vascular Surgery.
Thirdly for operative treatment the Center can dispose of :
7 Operationtheaters (5 aseptic theaters, 2 for operations of infectious diseases)
Intensive Care Unit with14 Beds
Patient ward with modern 1-3 bed-rooms, TV, bath and shower, opened in 2008.
Digitale Bronchoscopy- Units (Oympus) with digital storage- and documentation-system.

The Interdisciplinary Intensive Care Unit
Contacts and care for foreign patients are organised by the Bureau for International Medical Contacts.
To allow an advance review of all medical documentation, examinational results and pictures, these can be sent in by postal mail, air mail, e-mail or courier. The fastest way is communication via a-mail.
Our secretary can be reached from Monday to Thursday from 8 a.m. to 5 p.m. and on Fridays from 8 a.m. to 2 p.m.
Tel.: from Germany 04221/ 99 4263, from other countries: 0049/ 4221 – 99 4263
FAX: form Germany 04221/ 99 4265, other countries: 0049/ 4221 – 99 4265
e-mail: m.teschner@jh-del.de
Essential Requirements are
- a general condition and lung function of sufficient quality,
- the technical posibility to perform a resection,
- the oncological indication of an operation in case of a malignant disease (“oncologic indication”means the sense in an operative treatment according to the growth of a malignant tumor, the possibility of affected lymph nodes and metastasis),
- the consent of the patient to diagnostic and therapeutic procedures as well as the transmission of data.
To evaluate the severity of a disease and the possibilities to treat it, we need essential information beforehand. These include:
- 1. A complete personal history of the patient with relevant sicknesses und operations
- 2. Up to date results of clinical examinations, blood tests and an evaluation of the patients general condition including an estimate of his or her capacity do undergo a surgical procedure
- 3. Electrocardiography (ECG)
- 4. Analysis of blood gases and lung function (Bodyplethysmography/Spirometry)
- 5. Original pictures of imaging of the chest
(CT with contrast / MRI / PET-CT-Scan / X-Ray)
In case of a malignant disease, such as bronchial carcinoma, we also need
- 1. CT-Imaging of the head and
- 2. Scintigraphie of the skeleton
- 3. Results of biopsies or zytological examinations, if performed
In case of cardiac diseases additional examinations are necessary, such as
- 1. Echocardiography
- 2. Ergometry (ECG under physical stress)
- 3. Coronary Angiography in case of coronary stent-implantations, bypass-operations or similar procedures in the personal history.
Patients with mediastinal diseases are asked to send in pictures of magnetiv resonance imaging (MRI). If this is not possible a CT-Picture (with contrast) may suffice.
In certain cases additional examinations are necessary to plan an operation, these can be a bronchography (in case of bronchiectasy), spiroergometry (to evaluate the capacity of patients with severe obstructive and restrictive bronchial diseases) or an x-ray-imaging of the esophagus (if an esophageal involvement is suspected).
The preliminary evaluations of the possibility and good chances of operative treatment are free of any charge.
Costs for operative treatment (including the operation, preoperative examinations, postoperative monitoring, accomodation) vary according to the extent of the procedure.
We ask all patients, to check the coverage of the costs with their health-insurance and provide a written confirmation. If needed, an estimate of the expected costs can be given.
Payment and all financial transactions will be in Euro.
The Center is situated in Western Europe -> Germany -> Lower Saxony in the North of Germany -> Delmenhorst (near Bremen).
How to get to us by car
Coming from Bremen take the A1 (direction of Osnabrück) until exit “Delmenhorst-Ost”, then get on the A28 (in the direction of Oldenburg) until the exit “Delmenhorst-Deichhorst”. Turn right at the autobahn-exit, the hospital is on the left hand side after ca. 500 meters.
How to get to us by train
Get of the train at “Delmenhorst-Hauptbahnhof” (Delmenhorst main station), exit the station to the bus terminal (“ZOB”). Take the bus line Nr. 201 and exit at the bus stop „Wildeshauser Straße/ Krankenhaus“ directly in front of the hospital.
How to get to us by bus from Bremen
At the bus terminal beside Bremen main station take the Bahnbus to “Delmenhorst- Hauptbahnhof”. Change there to bus line Nr. 201 and exit at the bus stop „Wildeshauser Straße/ Krankenhaus“ directly in front of the hospital.

Natural and comforting area surrounding the Josef- Hospital Delmenhorst.

The hospital premises with forest and meadows.