 Information for professionals
Information for professionals
Information for Patients
In April 1928 the “Städtische Krankenanstalten”, the communal hospital of Delmenhorst, was opened. The facility included not only a farm to provide self-grown food, but also the first regional “Infektionshaus”, a clinic for the treatment of infectious diseases. Mainly patients suffering from tuberculosis, a widespread disease also called “white plague”, were looked after in generous buildings, called pavillions, with wide balconies, providing excellent conditions for the treatment.
At the end of the second world war the population of Delmenhorst multiplied and the hospital had to be extended. The introduction of effective antitubercular medication led to a decrease in patient numbers, but at the same time more and more patients suffered from lung cancer (carcinoma) or malignant diseases of the pleura (mesothelioma) due to growing cigarette consumption after the war and an occupational exposition to asbestos in the wharves and the ports of the area, the danger of which was not known at that time.
This resulted in a growing need for medical therapy of pulmonary diseases in Delmenhorst.
Other benign diseases of the airways, like asthma, traumatic injuries and all kinds of infections, had to be treated frequently. Further development of non-surgical pulmonary medicine also led to advances in anaesthetic and surgical technique, allowing the removal of lung tumors and the control of complications, for example thoracic infections. This caused the establishment of thoracic surgery as a specialist field of general surgery.

Pic. 1: Josef- Hospital Delmenhorst, Lower Saxony (Germany); the oldest building opened in 1928.
Presently the Center for Thoracic Surgery and Intrathoracic Vascular Surgery attends to ca. 620 patient (inpatients and outpatients) per year with an annual increase of 20%. In 2007 a total of 349 patients were given operative treatment. Of these operations 38% were performed using minimal invasive techniques (“key hole procedures”). In 52% an approach of 8-10 cm length, just below the breast muscle was used and in 10% a combination of minimal invasive technique with conventional procedure was applied, a new method developed in this hospital. The average stay was 7,9 days long with an intensive care treatment of 1,3 days (in case of extensive lung resections).
Complication rates were very low, the mortality rate for the resection of lung lobes (lobectomy) was 0% in 2007 (average in Germany 1-4%), for the resection of a lung wing (pneumonectomy) was 0.3% (average in Germany 6-17%) and for more extensive operations including the heart 0.9% (average in Germany 8-19%). The rate of general complications was 1,8% over all operations. The most common problem was a transient pneumonia following the operation.
The Center for Thoracic Surgery and Intrathoracic Vascular Surgery includes three major facilities:
The new patient wards, opened in 2008, with spacious, comfortable rooms, modern sanitary facilities, TV and radio in every room.

Pic 2: Center for Thoracic Surgery, newest building, opened in 2008.

Pic. 3: Reception area of ward C2 (thoracic surgery).

Pic. 4: Patient rooms, spacious and friendly, equipped with facilities for physically handicapped persons.

Pic. 5: Lounge of ward 31 (thoracic surgery).
The north wing of the old building was converted to a modern outpatient clinic, conserving the architectural details.

Pic. 6: Outpatient clinic of the Center for Thoracic Surgery and Intrathoracic Vascular Surgery.
For the surgical treatment the Center for Thoracic Surgery and Intrathoracic Vascular Surgery can dispose of adequate capacities in the modern intensive care unit, the operation theatres und the department for endoscopy.

Pic. 7: The Interdisciplinary Intensive Care Unit.
A team of specialists is prepared to treat patients with all kinds of thoracic diseases:

Pic. 8: Prof.HUST WuhanDr.med. Martin Teschner specialist for general, thoracic and vascular surgery and medical director of the Center for Thoracic Surgery and Intrathoracic Vascular Surgery
(e-mail: m.teschner@jh-del.de)

Pic. 9: Frau Iris Martens, chief secretary of the Center for Thoracic Surgery and Intrathoracic Vascular Surgery
Tel.: 0049/ 4221 – 994263; FAX 0049/ 4221- 994265.
Pic. 10: Herr Dr.med. Matthias Esch
Specialist for general surgery and assistant medical director.

Pic. 11: Dr.med. A. Müller, psychooncologist; specialist for the psychological assistance to patients with malignant diseases.

Pic. 12 and 13: The nursing team of ward 31 (thoracic surgery)


Pic. 14: Specialised and experienced in the care for patients of thoracic surgery: the nursing team of ward.

Pic. 15: The team of the department for physiotherapy.
The Center of Thoracic Surgery and Intrathoracic Vascular Surgery can dispose of all modern technical methods surgical therapy, including minimally invasive procedures (“key hole-technique”), Laser- or Argon-Beamer carbonisation, vascular replacements and digital bronchoscopy.
All other than pulmonary affections are specially looked after by an interdisciplinary network of internal, pneumological, cardiological and anesthesiological therapists. Severe conditions are treated by the team of our intensive care unit. Patients with highly contagious diseases are cared for in a special unit for infectious diseases.
Very important for all operations are techniques to conserve lung tissue to achieve a maximum of pulmonary function after a resection has been performed. To that end modern methods of tissue-sparing resections and vascular replacement are regularly employed, allowing the conservation of functioning lung tissue, which otherwise would have to be removed. The quality of life after a tissue-sparing operation is significantly better, because the physical capacity is less incriminated. Methods of vascular surgery can also be used to treat congenital or acquired malformations of blood vessels. For that reason the department for thoracic surgery has been combined with the clinic for vascular surgery to form the Center of Thoracic Surgery and Intrathoracic Vascular Surgery.
New developments of the Center of Thoracic Surgery and Intrathoracic Vascular Surgery are procedures combining classical surgical and minimally invasive techniques, called “interventional surgery”. By using these methods of interventional surgery only small skin cuts are needed even for large resection, reducing the physical stress of the operation (pic. 16 und 17).
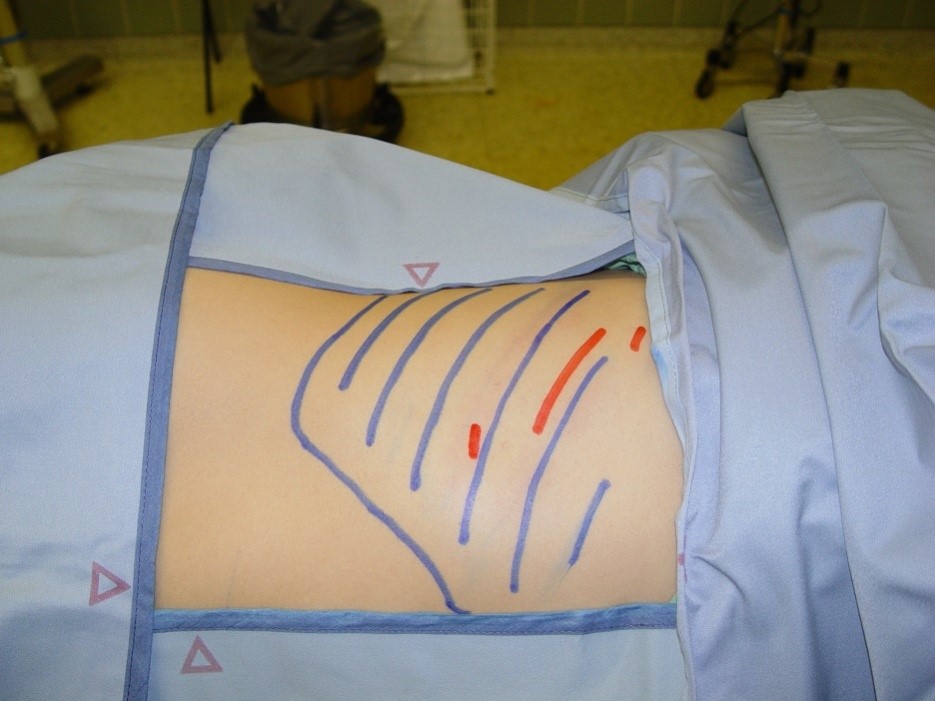
Pic. 16: Size and localisation of the skin cuts fort he performance of a thoracic operation using classical technique (blue marks) or combined with minimally invasive methods (red marks).

Pic. 17: Small wounds and cosmetically favourable approach to a lung operation (here a 26 year old patient, 21 days after the resection of destroyed parts of the lung).
The Center of Thoracic Surgery and Intrathoracic Vascular Surgery has also developed several methods for the treatment of disorders of the diaphragma or its nerves.
Because the diaphragma is the most important muscle in breathing, its paralysis can cause a severe impairment. The proper function of the diaphragma can be restored using our new procedures.
A. Operative procedures are performed on
Children (5 years and older) and adults (regardless of age) suffering from
- Tumors of the airways, the lung or the mediastinum, such as
- a. Bronchial or tracheal carcinoma
- b. Metastasis
- c. Benign or malignant pleural tumors (e.g. mesothelioma)
- d. Benign or malignant tumors of the thymus gland
- Intrathoracic infections with empyema or abscess
- Effects of traumatic lesions
- Cysts or bullae (pulmonary emphysema)
- Residual symptoms of tuberculosis
- Congenital anomalies (e.g. bronchiogenic cysts, anomalies of blood vessels or lung tissue)
- Lesions and diseases of the trachea
B. No operations are performed on
- Patients with cardiac diseases necessitating the use of a heart-lung-machine (e.g. cardiac bypass operations or cardiac valve implantations);
- Vascular Alterations of the central Aorta (from the heart to the branch of the artery supplying the left arm).
The implantation of small catheters allows a continious spinal application of analgetic medications for the efficient control of postoperativ pain.
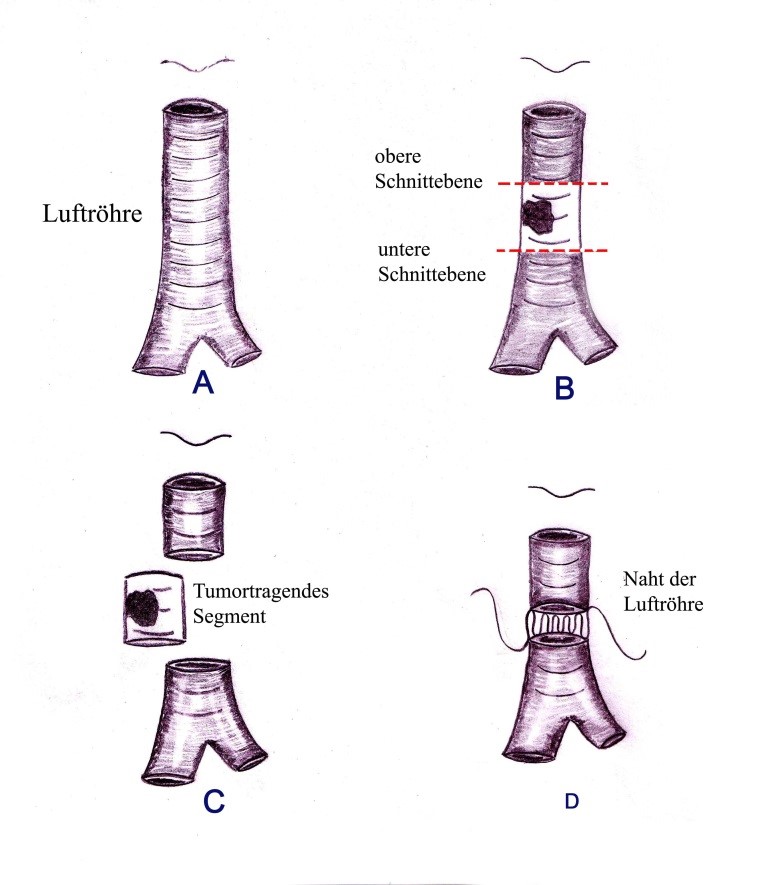
Pic. 18: Example of the resection of a tumor of the windpipe. After the tumorbearing segment has been removed, the ends are united using special sutures.
Contacts and care for foreign patients are organised by the Bureau for International Medical Contacts.
To allow an advance review of all medical documentation, examinational results and pictures, these can be sent in by postal mail, air mail, e-mail or courier. The fastest way is communication via a-mail.
Our secretary can be reached from Monday to Thursday from 8 a.m. to 5 p.m. and on Fridays from 8 a.m. to 2 p.m.
Tel.: from Germany 04221/ 99 4263, from other countries: 0049/ 4221 – 99 4263
FAX: form Germany 04221/ 99 4265, other countries: 0049/ 4221 – 99 4265
e-mail: m.teschner@jh-del.de
The preliminary evaluations of the possibility and good chances of operative treatment are free of any charge.
Costs for operative treatment (including the operation, preoperative examinations, postoperative monitoring, accomodation) vary according to the extent of the procedure.
We ask all patients, to check the coverage of the costs with their health-insurance and provide a written confirmation. If needed, an estimate of the expected costs can be given.
Payment and all financial transactions will be in Euro.
The Center is situated in Western Europe -> Germany -> Lower Saxony in the North of Germany -> Delmenhorst (near Bremen).
How to get to us by car
Coming from Bremen take the A1 (direction of Osnabrück) until exit “Delmenhorst-Ost”, then get on the A28 (in the direction of Oldenburg) until the exit “Delmenhorst-Deichhorst”. Turn right at the autobahn-exit, the hospital is on the left hand side after ca. 500 meters.
How to get to us by train
Get of the train at “Delmenhorst-Hauptbahnhof” (Delmenhorst main station), exit the station to the bus terminal (“ZOB”). Take the bus line Nr. 201 and exit at the bus stop „Wildeshauser Straße/ Krankenhaus“ directly in front of the hospital.
How to get to us by bus from Bremen
At the bus terminal beside Bremen main station take the Bahnbus to “Delmenhorst- Hauptbahnhof”. Change there to bus line Nr. 201 and exit at the bus stop „Wildeshauser Straße/ Krankenhaus“ directly in front of the hospital.

Pic. 20: Natural and comforting area surrounding the Josef- Hospital Delmenhorst.

Pic. 21: The hospital premises with forest and meadows.